What is Fructose Intolerance?
Disclaimer: I am not a nutritionist, dietician, or scientist. I am a teacher and a graduate student who spent years struggling with my own digestive and gastrointestinal health. My goal is to share what I have learned across dozens of doctor’s appointments, countless hours of research, and too many medical tests to count.
There is a growing occurrence of dietary fructose intolerance, also referred to as fructose malabsorption. At a basic level, this means that a person cannot properly digest fructose, so consuming foods with high amounts of fructose can lead to numerous unpleasant symptoms. Dietary fructose intolerance can develop at any age. This is different from hereditary fructose intolerance, which is much rarer and occurs when a person produces none of the enzyme needed to digest fructose, aldolase B (symptom onset as a baby). While hereditary fructose intolerance can be life-threatening, dietary fructose intolerance leads to milder but still significant symptoms: severe bloating and distension (episodic or long-term), gas, diarrhea, belching, abdominal discomfort, and more. Many of these symptoms overlap with those of IBS and SIBO (small intestinal bacterial overgrowth), so it may be unclear when to examine fructose intolerance as the underlying issue. One study (Choi et al., 2008) estimated that as many as 1/3 of patients diagnosed with IBS might actually be struggling with fructose intolerance.
What is fructose?
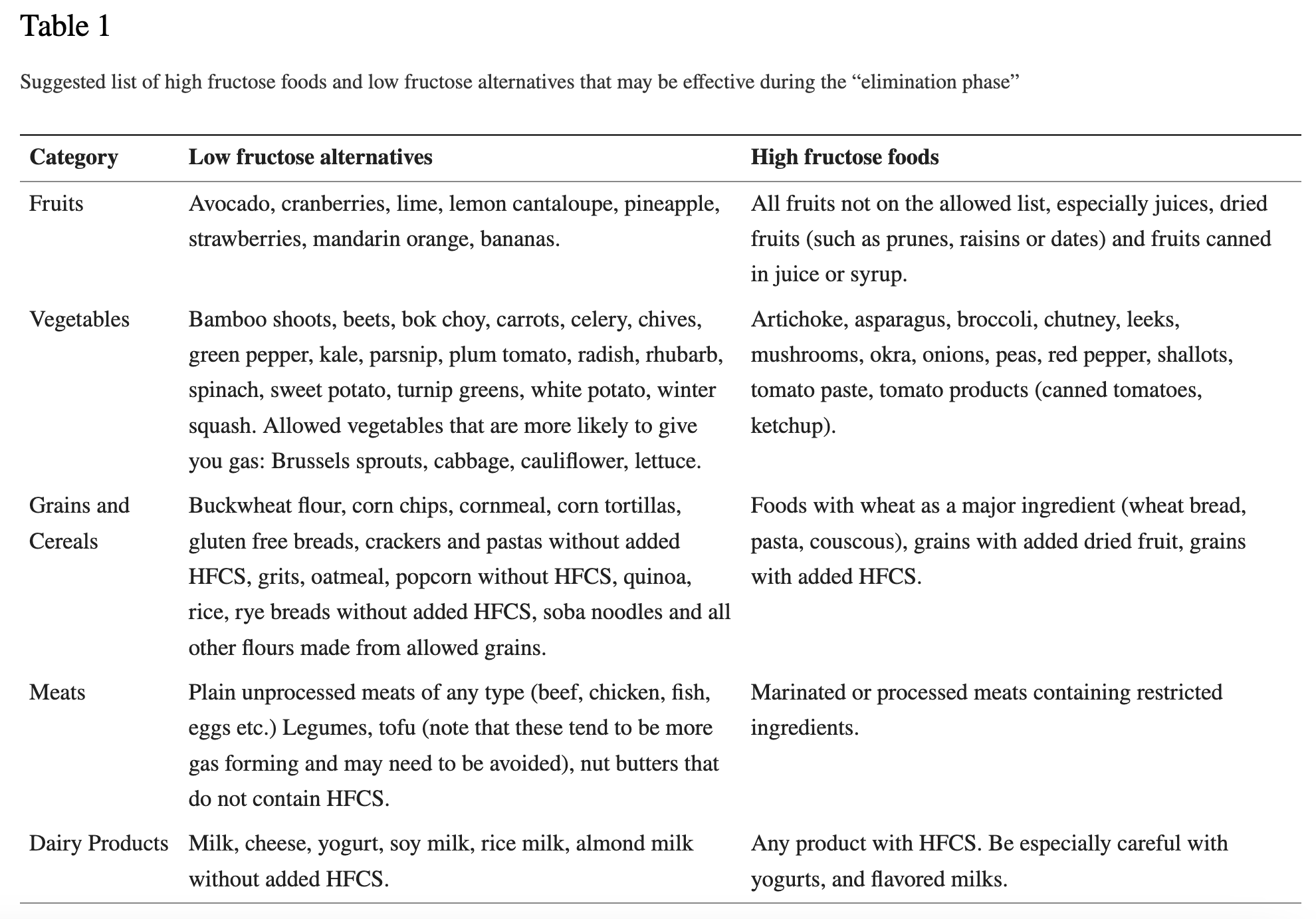
Fructose is a type of monosaccharide (the “m” in FODMAPs) that is sometimes called “fruit sugar.” Despite that moniker, fructose is not only found in fruit—it is common in many vegetables and in sweeteners such as honey, agave, and high-fructose corn syrup. Fructose consumption has risen dramatically in the past few decades, in large part due to the prevalence of high-fructose corn syrup. The following table from Fedewa and Rao (2014) provides an overview of foods high and low in fructose.
The gist: If you don’t produce enough of the enzyme aldolase B or your intestines cannot digest fructose properly, foods you eat that contain fructose can’t be digested properly and sit around in your gut, fermenting and causing serious bloating, gas, and digestive issues. According to WebMD, your ability to digest fructose can also be impacted by conditions like Celiac disease, Crohn’s disease, gastroenteritis, inflammation, stress, and antibiotic use. My own gut issues started after several consecutive illnesses that required antibiotic and steroid use.
How do I know if I have fructose intolerance?
Similar to the test for SIBO, fructose intolerance is diagnosed with a breath test. First, you discontinue any medications or supplements that would interfere with the test, and you complete a 24-hour highly restricted diet (basically, plain chicken, plain rice, plain white bread, plain eggs, and water). After a 12-hour overnight fast, you take a baseline measurement by blowing into a special tube. Then, you drink a solution of fructose mixed with water. If you’re like me, you blow up like a hot air balloon at this point. Not everyone reacts this quickly, so no symptoms doesn’t mean you’re negative for FI, and sometimes severe symptoms during the test can lead to a diagnosis even if the measurements are unclear. Over the next few hours, you continue to fast and blow into a tube every hour so that a doctor can identify what your digestive system does after consuming the fructose.
Note 1: Interestingly, despite my very strict adherence to the restricted diet and fasting regime, my doctor had to call to confirm if I’d followed the directions. Apparently, the fructose built up in my system was so significant that, even after the fructose-free diet and fasting, my baseline measurement was still really high.
Note 2: Based on my research, SIBO and fructose intolerance commonly co-occur. The typical pathway is to diagnose and treat SIBO first (which I did). If symptoms recur down the road (which mine did), then you explore whether the SIBO has returned or if you should also be tested for fructose intolerance. Fructose intolerance also frequently cooccurs with other intolerances (lactose, sucrose, sorbitol, etc.).
Note 3: If you have not been diagnosed with fructose intolerance, then cutting fructose out of your diet probably isn’t a healthy choice. Many healthy foods contain fructose and should only be limited or eliminated if you can’t tolerate them.
Limiting Fructose
If you are diagnosed with fructose intolerance, the main solution is to limit your fructose intake. Unlike some other intolerances where you can take a pill that helps replace the enzyme you need, no such solution exists for fructose intolerance (yet). There are some products that include other enzymes (like xylose isomerase) that supposedly help with converting excess fructose to glucose, which is easier to digest (more research is needed about if this actually helps with FI symptoms). However, as far as my doctors and I know, there is no aldolase B supplement. Basically, you just have to try to really limit your fructose intake so that your body can keep up with digesting it.
Consuming zero fructose is basically impossible and would require a highly, highly restrictive diet. Rather, the goal is to reduce fructose intake as much as possible and establish how much you can tolerate. It is important to continue eating fruits and vegetables in ways that your body can handle. One guideline I’ve seen a few places is to try to keep your fructose content under 3 grams per serving. The challenge is that there are inconsistent and incomplete resources regarding how many grams of fructose are in different foods. It gets even more complicated when you learn about glucose-to-fructose ratios and free fructose (another blog coming soon). Because you have to eliminate or restrict so many fruits and vegetables, it is a good idea to supplement with a multivitamin.
Note: Because there may be a large buildup of fructose in your system, it may take a while to start feeling better and seeing your symptoms subside after switching to a low-fructose diet. It was at least several weeks and maybe closer to two months before my permanent bloating really started to get better, but flare-ups of my other symptoms improved much more quickly.
According to Fedewa and Rowe (2014), “There are no established protocols or guidelines in the dietary management of fructose malabsorption or intolerance.” That means that trial and error are about to be your best friend. Future blog posts will address how to do a fructose elimination diet, how to reintroduce certain foods, and how to manage fructose intolerance long-term. Unfortunately, fructose intolerance and fructan intolerance are often related, so that topic will be explored as well.
References
Fedewa & Rowe (2014): Dietary Fructose Intolerance, Fructan Intolerance and FODMAPs
Hedge & Sharman (2023): Hereditary Fructose Intolerance
WebMD (2021): What is fructose intolerance?